Lupine Publishers | Journal of Pediatric Dentistry
Abstract
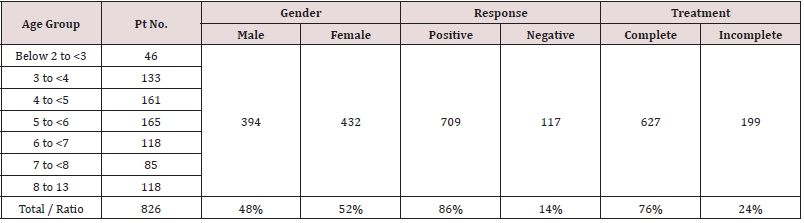
Fissure sealant is one of effectual method for prevent occlusal caries. Therefore, removing contaminated organic debris and plaque was important process to attain sufficient sealant retention. The aim of this study was revaluated the cleaning method and invasive technique to an occlusal fissure. Twenty-four teeth with deep fissure were used in this study and 15 teeth were cleaned by finger spreader, bristle brush and ultrasonic scalar, respectively. Remain 9 teeth were prepared fissure groove using three kinds of minimal intervention burs (BR-48, CD-50F and CD-53F). The ratio of remaining debris by fingers spreader, bristle brush and ultrasonic scalar were 35 %, 65%, 25% respectively. In contrast, each fissure with invasive technique was not observed residual debris. The average preparative fissure groove by BR-48, CD-50F, CD-53F were 1.38mm, 1.40mm and 0.76mm in width, and 1.58mm, 1.66mm, 1.18mm in depth, respectively. From these results, invasive technique as fissure pretreatment before acid etching might be effective to success for good fissure sealant retention for a deep and narrow fissure and a CD-53F bur was most less preparative sound enamel.
Keywords: Fissure cleaning; invasive technique; fissure sealant
Introduction
Immature permanent teeth have a risk of occurring dental caries. Especially the percentage of occlusal pit and fissure caries is over 80% of all caries in immature permanent teeth [1]and Carlos JP et al. reported that a high percentage of these occlusal lesions occurred the caries in the first 3 years after tooth eruption [2]. Dental plaques and organic debris are easy to accumulate in a pits and fissure of occlusal surface in immature young permanent teeth, and those plaque and debris were hard to remove from pit and fissure completely by ordinal cleaning method such as using low speed of rotary tooth brush. Therefore, a technique by capping of fissure with fissure sealant is widely used in ordinal dental clinic for preventing occlusal caries. However, fissure sealants are occasionally removed out partially or totally from fissure for a long term of retention. Complete or partial fissure sealant retention after 8-10 years was reported by some studies [3-5]. The main reason of them seems that fissure sealants are not able to penetrate into whole of fissure for the characteristic of narrow fissure and prevention by dental plaques remaining into a bottom of pits and fissure. Therefore, complete removal of debris and plaque are important factor for success of fissure sealant. Although conventional technique with rotary brush was commonly used by clinical dentist, there is a possibility of remaining dental plaque or organic debris in a pits and fissure with this treatment. The shape of fissure groove might influence on disturbing fissure cleaning. Because fissure are deep and narrow in immature molar teeth typically and it is hard to attach cleaning instrument to those debris and they are staying in the bottom of fissure for long period Moreover deep and narrow shape of fissure is disadvantage for penetrating of fissure sealant into whole of fissure groove. Therefore some researchers insist that invasive technique as enamel pre-treatment by fissure bur [6-9], air abrasion [10,11] or laser [12,13] before enamel etching and fissure sealing are necessary to success of cleaning of pits and fissure and penetration of fissure sealant sufficiently. However, these invasive techniques are not widely acceptable for young teeth treatment and there has still discussed whether invasive pre-treatment is necessary for fissure sealants or not [14-17]. Therefore, this study is investigated that the debris removing ability from noninvasive pit and fissure were using several kinds of cleaning methods such as conventional rotary brush, ultrasonic scalar, chemically agent. Furthermore, invasive techniques as a fissure pre-treatment were also investigated using several minimal intervention burs.
Materials and Methods
Sample corrected and preparation
Twenty-four extracted human permanent molar and wisdom teeth with deep pit and fissure were used in this study. Following an approval of use for this study by the patients, those teeth had checked their depth of fissure by dental photography and adapted similar condition of fissure were used in this study. Furthermore, they had no caries in occlusal surface. Before research, all teeth were cleaned by brushed and washed with distilled water and stored at room temperature.
Application of artificial organic debris into fissure groove
To specific valuation of removing debris ability, each fissure of all experimental teeth was filled with artificial organic debris. The organic debris was prepared according to a previous report [18]. It contained 20% of Liquitex (Liquitex Co., USA), 30% of Starch gruel (Fueki-ko, Fueki Co., Yao, Japan), 30% of Poster color (Sakura Co., Osaka, Japan), and finally 20% of solid food fragments for rats (MR-stock, Nihon-Nosan Co., Yokohama, Japan) originally used for animal feed. All ingredients were mixed together to simulate a clinical debris condition. All specimens were then stored in a moist chamber until start study.
Group classification
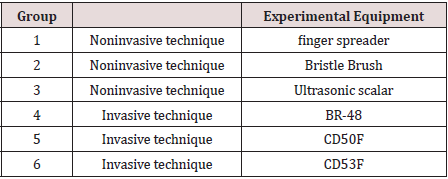
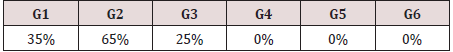
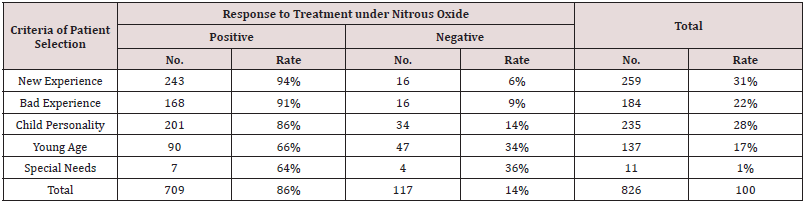
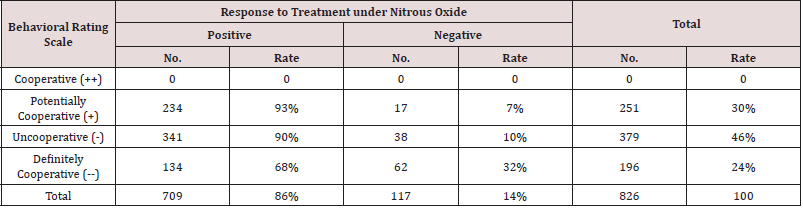
All specimens were classified into 6 groups at randomly according to the difference of cleaning method or fissure pretreated burs. Each 5 teeth were elected in group 1 to group 3 respectively (15 teeth) and those teeth were evaluated several cleaning methods without fissure invasive technique. Group1 was cleaned fissure by hand instrument (finger spreader). Group 2 was used bristle brush to fissure cleaning. Group3 was performed fissure cleaning by ultrasonic scalar. Remaining 9 teeth were divided into 3 groups (Group4 to 6) in each 3 teeth. These three groups were applied invasive technique using several types of fissure preparative burs. The detail of this classification was shown in Table 1.
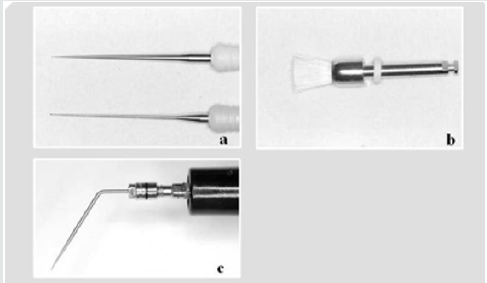
Experimental Procedure for noninvasive fissure
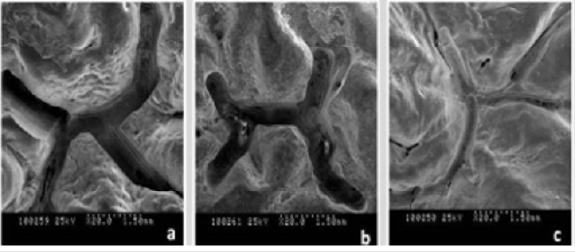
In Group 1, fissures were cleaned with finger spreader (Mani Inc Tochigi, Japan). The fissures were gently excavated with a 15- size flare finger spreader using a vibratory motion and rinsed with water spray. This process was continued until the debris was removed completely from the fissure groove (Figure 1a). In Group 2, fissures were cleaned by pointed bristle brush (Merssage brush CA, YDM Co, Tokyo, Japan) with water spray. Bristle brush was setting in a low-speed handpiece (550 cycles per minute) and leaning procedure was performed for 30 seconds. All teeth were then dried with oil-free compressed air for 20 seconds and subjected to the following investigations (Figure 1b). In Group 3, fissures were cleaned with ultrasonic scalar with thin tip (ENAC, SC point 4, OSADA Inc Tokyo, Japan) under water spray condition. Scalar head were touched and moved with the fissure groove gently and continue procedure until artificial organic debris removing (Figure 1c). Even organic debris was not removed completely, cleaning procedure using above each method was stopped within 30 seconds. Then each fissure was observed by stereomicroscope to check the ratio of residual debris.
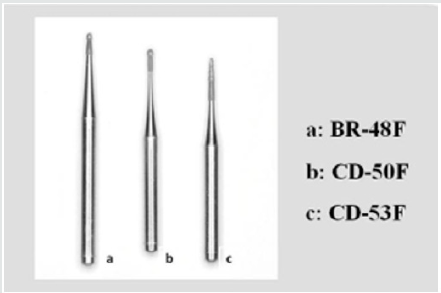
Fissure preparation for invasive technique
Remain 15 teeth were used for invasive technique. After each fissure groove were washed, then fissure groove was prepared by three types of diamond burs. Type 1 and type 2 were small round diamond burs (BR-48 and CD-50F). Type 3 (CD-53F) were fissure type diamond bur. These all burs were produced for Minimal Intervention (MI) and are especially designed to prepare the cavity minimally as possible. These burs were connected with high speed hand piece and keep the speed as a 3000 rpm during fissure preparing procedure (Figure 2).
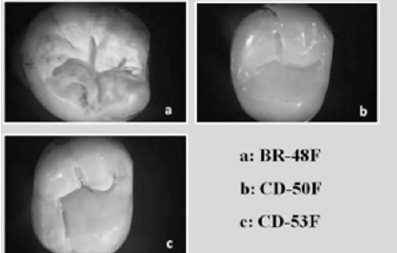
Stereoscope and SEM observation of invasive fissure
To verify the surface characteristics, each 3 teeth in group 4 and group5 (total 6 teeth) were selected randomly and fissure condition after invasive technique were examined using a stereomicroscope (SMZ-10, Nikon, Tokyo, Japan). Following stereomicroscopic observation, and then followed by scanning electron microscopic (SEM) examination. For SEM examination, specimens were dehydrated with a graded series of aqueous ethanol (70%, 80%, 90%, and 100% ethanol) for 24 hours in each solution, dried with liquid CO2 using a critical point dryer device (JCPD-3, JEOL, Tokyo, Japan), coated with a platinum layer to a thickness of 15 μm, and observed by SEM (JSM-T220A, JEOL) at 15 kV.
Results
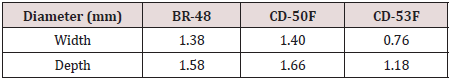
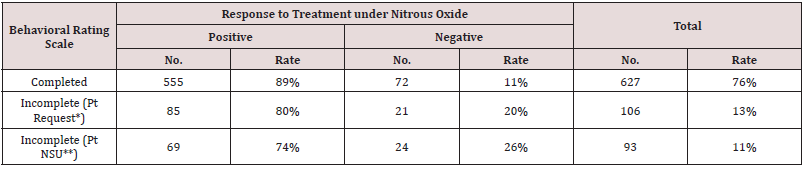
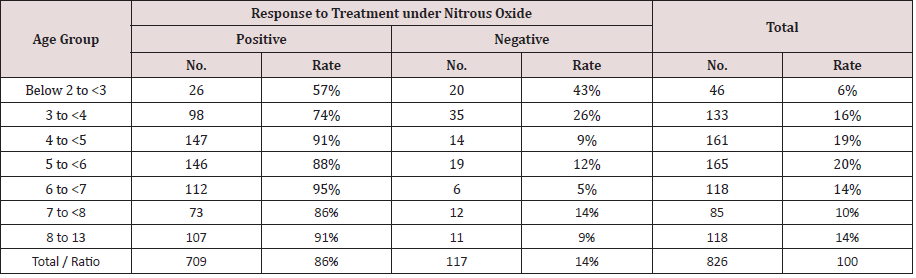
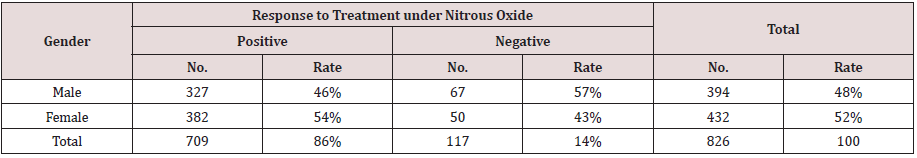
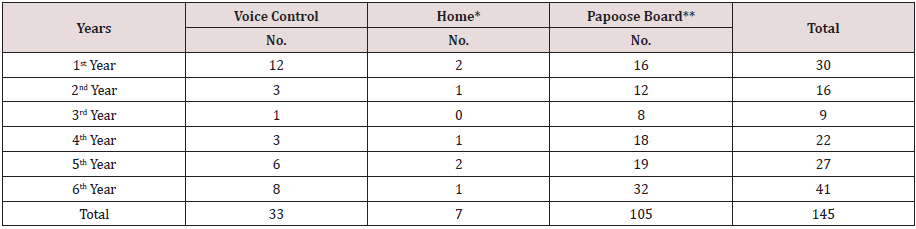
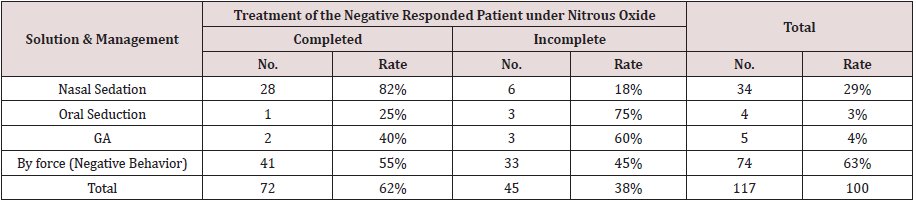
The evaluation of each fissure preparation by several kinds rotary bur
Figure 3 showed the condition of after pretreated fissures in invasive technique groups by stereoscopic observation. There was not revealed an abnormality mentioned such as a tooth fracture, tooth crack in all teeth. Scanning electric microscopic observation indicated that the pretreated fissure by the bur of CD-53F made most shallow and narrow fissure shape in three kind’s diamond burs (Figure 4). The width of invasive fissure of BR-48F, CD-50F, CD-53F were 1.38mm, 1.40mm, 0.76mm respectively. The average of depth of invasive fissure of BR-48F, CD-50F and CD-53F were 1.58mm, 1.66mm, 1.18mm respectively. Total results by fissure preparation by each diamond bur indicate in Table 2. The ratio of residual debris by each cleaning method both noninvasive fissures and invasive fissures. In the groups of normal fissures showed 25 % of debris was residue in ultrasonic scalar groups. In contrast, 35% and 65 % debris were not removed out from fissure by finger spreader and bristle brush, respectively. In 3 gropes with invasive technique to fissure, all debris was removed completely from fissures (Table 3).
Discussion
To attain fissure sealant, penetrate into pit and fissure completely, the process of fissure cleaning that cause free of gross plaque and debris is important key for success of fissure sealant application. This study demonstrated that several fissure cleaning techniques using finger spreader, bristle brush and ultrasonic scalar, had not success of dental organic debris removing completely in non-inversed fissure. Remaining organic debris was mainly present on the deep narrow fissure wall and bottom of the fissure groove. These results supported that previous several similar researches that compared with both bristle brush cleaning and mechanical fissure preparative cleaning. They suggested that remaining debris and pellicle were not removed from the bases of fissures by routine cleaning and etching procedures [19-21]. Therefore the reason of remaining debris of noninvasive fissure groups in this study should be the entrance to shallow and wide groove of fissure were easy to remove debris by ordinal cleaning instruments, conversely the deep fissure wall and bottom of fissure groove were not able to attack by cleaning instrument directly. Thereby many organic debris were not removing from fissure and remaining deep side fissure wall and bottom of groove even carried out several fissure cleaning techniques using finger spreader, rotary bristle brush and ultrasonic scalar. Many cases of these phenomenon were occurred by not only relate fissure depth, but also fissure width.
These types of fissure were inhibiting fissure cleaning effectiveness, and it cause insufficient etching agent and sealant penetration, and consequently reducing adaptation ability and easy to lack of retention of sealant are occurred. From this evidence, invasive technique as a fissure pre-treatment was effectiveness to both fissure cleaning and sealant penetration. Many researchers proposed that mechanical invasive technique has good advantage for fissure sealant retention [22,23]. The result of several in vitro studies on the invasive technique with mechanical preparation has indicated that the risk of microleakage is reduced when the fissure is preventively enlarged with rotating burs [24-26]. Shapira and Eidelman have shown higher retention rate in vivo with the use of a #1 round steel bur at low speed after 6 year, compared to non-mechanically prepared fissures [27,28]. Lygidakis et al. suggested their clinical study in observed for four years that the mechanical preparation of occlusal surface offer sealant retention [29]. Even these studies have demonstrated, still several researchers insist that invasive techniques were not necessary for fissure sealant application. Blackwood JA et al. reported that there was no significant difference in microleakage between the fissure cleaning with traditional pumice prophylaxis technique, fissure invasive technique and air abrasion technique [30]. However, its studies were evaluated by microleakage test using thermal cycling procedure within dwelling 500 cycles. Previous Yamada et al compared sealing ability of fissure sealant both Carisolv-and bristle brush-treated using microleakage test with 400 cycles thermal cycling [18]. Their result demonstrated that the fissure treated with bristle brush showed remaining organic materials in the bottom of groove. However, the results of microleakage tests were not specific difference both the group of removing debris completely and the group of remaining debris in bottom of the fissure.
They discussed the possibility of that the fissure sealant may have maintained a high sealing effectiveness to the marginal side wall even debris was not removed and remaining on the deep side wall in the fissure during microleakage test procedure. Therefore, microleakage test may not be a reliable evidence for the decision whether fissure pretreatment before etching and fissure sealant application is necessary or not. Accordingly sealing force of sealant was significantly reduce according passage of time and this situation might has a possibility of causing occlusal caries when it is occurred the detach or fracture of fissure sealant, and the debris which are contaminate several bacteria penetrate into bottom of the fissure. Although invasive technique is a good method for sealant retention, this technique should not necessary to transact for all pit and fissure. It must be selected for only hardness to debris remove completely by ordinal technique such as bristle brush and prophylaxis paste and prepared for only broad narrow fissure sharp fissures. De Craene et al. has also similar suggestion, they proposed that in a tooth with open fissures, not suspected of being carious, a prophylactic treatment for non-invasive pit-and-fissure sealing technique should be chosen, by contrast in case of deep and narrow fissures that are discolored and suspected of being carious, the invasive pit-and-fissure sealing technique should be chosen [22]. Welbury et al. reported that purposeful invasive technique just to widen the base of a fissure in a sound tooth is an invasive technique, which disturbs the equilibrium of the fissure system and exposes a child unnecessarily to the use of a handpiece or air abrasion [30]. Therefore, they insisted that invasive technique for occlusal fissures was not necessary and undesirable method. To resolve this doubtful problem, invasive technique must be performed most minimal preparation as possible.
This study was also investigated the invasive technique, then evaluated the instruments for fissure pretreatment both fissure type and round head diamond point bur which were produced for minimal intervention. Present results demonstrated that round head diamond point bur made causing unacceptable width and depth fissure sharp, because it seems round head diamond bur was smoothly moving and control was not easy to keep a fissure external form consequently fissures became more wide and deeper than what was assumed. Conversely, fissure type of diamond bur caused minimal fissure groove and it might be acceptable depth and width of them. This research proposed that CD53F fissure head diamond bur that was used in this study may good candidate for fissure preparation instrument and Garcia-Goddy et al. also recommended fissure type diamond point bur (Sorensen bur) [7]. From this result and previous those results, the fissure type diamond point may most acceptably instrument for invasive technique. The results of present study strongly suggested that the important factor for success of fissure sealant should select a case of proper fissure whether invasive technique is necessary or not. In case of performed invasive technique to immature occlusal fissure, minimal preparation of fissure pre-treatment is the key for safety and sufficiently good retention of fissure sealant.
Conflicts of Interest
There are no conflicts of interest.
Read More Lupine Publishers
Pediatric Dentistry Journal Articles:
https://lupine-publishers-pediatric-dentistry.blogspot.com/