Lupine Publishers | Journal of Pediatric Dentistry
Abstract
This case report describes the management strategies and the
evolution of the acute herpetic gingivostomatitis condition in
a 3-year-old female child with a focus on suppressing pain and to
improve oral intake with approaches to medicine and dentistry.
Keywords: Herpect Stomatitis; Drug Therapy; Child
Introduction
Herpetic gingivostomatitis is a condition that most often results
from initial gingiva (gums) and oral mucosa infection with herpes
simplex virus type 1 (HSV-1). While herpetic gingivostomatitis is
the most common cause of gingivostomatitis in children before the
age of 5, it can also occur in adults. The condition is characterized
by a prodrome of fever followed by an eruption of painful, ulcerative
lesions of the gingiva and mucosa, and often, yellow, perioral,
vesicular lesions. HSV-1 is usually spread from direct contact or
via droplets of oral secretions or lesions from an asymptomatic or
symptomatic individual. Once a patient is infected with the herpes
simplex virus, the infection can recur in the form of herpes labialis
with intermittent re-activation occurring throughout life [1]. The
pathogenesis of herpetic gingivostomatitis involves replication
of the herpes simplex virus, cell lysis, and eventual destruction
of mucosal tissue. Exposure to HSV-1 at abraded surfaces allows
the virus to enter and rapidly replicate in epidermal and dermal
cells. This results in the clinical manifestation of perioral blisters,
erosions of the lips and mucosa, and eventual hemorrhagic
crusting. Sufficient viral inoculation and replication allow the virus
to enter sensory and autonomic ganglia, where it travels intraaxonally to the ganglionic nerve bodies. HSV-1 most commonly
infects the trigeminal ganglia, where the virus remains latent
until reactivation most commonly in the form of herpes labialis
[2]. While most children with primary gingivostomatitis will
be asymptomatic, some will experience considerable pain and
discomfort and are at risk of dehydration. There are no large, well
designed studies to clearly determine appropriate therapy for all
children [3]. Professionals who treat children in this age group
must be able to diagnose and treat common oral manifestations
when necessary and should refer the child to a pediatrician for
effective treatment if the presence of any systemic alteration is
suspected [4]. Herpetic infections commonly affect the dental
profession’s anatomical area of responsibility and the diagnosis
and management of such infections fall in the purview of oral
healthcare providers. To administer competent care to patients
with herpetic infections, clinicians must understand the disease, its
treatment, the impact the disease or its treatment may have on the
patient and the extent to which the presence of a herpetic infection
may impact on caregivers in the clinical process [5]. The purpose
of this case report was to describe the treatment recommended for
a child diagnosed with acute herpetic gingivostomatitis associated
with tonsillitis and the ways to suppress pain and to improve oral
intake from the perspective of medicine and dentistry.
Case Report
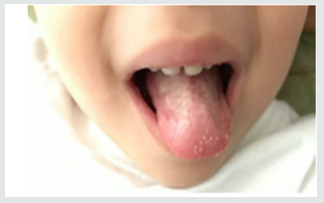
Parents of a 3-year-old and female child sought pediatrician
due to inflammation in the throat of their daughter, with fever and
irritability for two days, then their child feels pain in the mouth, and
the drooling starts with the appearance of diffuse lesions in the oral
mucosa, complaining of pain and having difficulty feeding. There
was the prescription of antibiotics (amoxicillin and clavulanate
potassium for oral suspension), anti-inflammatory and antipyretic.
Intraoral cleaning with gauze and saline was recommended and
the request for a new consultation, to eliminate the possibility of
fungal contamination. The diagnosis of acute and viral primary
herpetic gingivostomatitis was established (Figure 1). On intraoral
examination, gingiva appeared fiery red in color and multiple
vesicles were present on the attached mucosa. Multiple vesicles
and ulcers were seen along the lateral border and anterior surface
of the tongue. Both sided buccal mucosa revealed multiple vesicles.
Her parents also complained about his bad breath during this
period due to poor oral hygiene. Submandibular lymphatic glands
of the kid were enlarged [6]. The pediatric dentistry was consulted
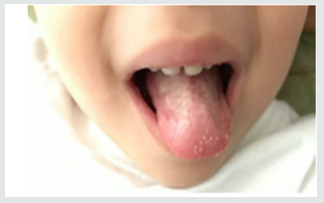
because the child persisted with much pain, unable to sleep or eat
(Figure 2). There was then the option of laser applications, with
faster healing of ulcers and greater pain relief. There was substantial
improvement in food, oral hygiene and sleep. The patient will
perform control examinations, with simultaneous evaluation by
pediatrician and pediatric dentistry.
Figure 1: Child oral examination two days under antibiotic prescription.

Figure 2: Aspect of the child’s tongue on the fourth day of drug treatment.