Lupine Publishers | Journal of Pediatric Dentistry
Abstract
Oral and dental health is of vital importance in children with cardiovascular system disease. Congenital and acquired heart diseases make oral treatment complicate in children and increase the risk of infective endocarditis [1]. The dentists main aim in children with heart disease should be to prevent infective endocarditis, to maintain periodontal health and to ensure a well oral hygiene. In these children, medical history should be taken in detail before dental treatment. Consult with the pediatrician and inform about the condition of the disease and the drugs used recently. Consideration should be given, and antibiotic prophylaxis should be evaluated consultation to in the treatment planning of children with heart disease. In these children, dental treatments should be performed quickly and effectively, and family awareness should be given importance [1-3]. In this review, common oral findings related to cardiovascular system diseases will be discussed and the precautions and treatment approaches of dentist will be mentioned [4].
Keywords: Endocarditis, heart diseases, intraoral findings, pediatric dentistry
Review
Almost all of the heart diseases seen in children are congenital. The most common structural congenital heart diseases are; ventricular septal defect, patent ductus arteriosus, atrial septal defect, fallot tetralogy, pulmonary stenosis, aortic coarctation, aortic stenosis and transposition of the great arteries. Large defects are surgically closed in the first years of life, and some defects may require complex surgical treatment and eventually transplantation. Acquired heart diseases such as myocarditis and infected endocarditis are the cause of disability and death in children [5]. Oral and dental health may be insufficient in children with congenital heart disease. The reasons for this; chronic vomiting in children up to one-year, dry mouth due to drugs used, neglect of oral care due to cardiac problems as the primary priorities of families [1]. Poor oral hygiene in children with heart disease may pose a risk for bacteremia. Infective endocarditis can result with severe valvular dysfunction, dehiscence, congestive heart disease and various embolisms leading to death. In the long term, it may cause cardiac valve damage and prosthetic regeneration of the heart valve [1,6-8].
Oral findings
Oral findings in children with cardiovascular disease include cyanotic gingivitis, stomatitis, glossitis, mucositis, cleft lip and palate, clefts in the tongue, the fungiform and filiform papilla of the tongue becoming dark red [5,9]. In addition, enamel hypoplasia, high incidence of caries, delays in teeth exfoliation, periodontal diseases and intrinsic discolorations are observed [5,9,10]. In particular, discolorations in permanent teeth occur due to the ingestion of blood and blood products by drugs, increased caries activity and poor oral hygiene [5]. Poor oral hygiene, use of drugs, inadequate food and mineral consumption are effective risk factors for the onset of periodontal disease in children with congenital cardiovascular disease [11,12]. Pourmoghaddas et al. [12] reported that children with congenital heart disease had significantly higher periodontitis than healthy children and that periodontal disease caused endocarditis risk. Al Alousi et al. [13] reported that the rate of development of enamel defects was high in patients with ventricular septal defect and was observed due to malnutrition. The researchers stated that nutrient elements may affect the epithelial cell function and mineralization process and prepare the ground for defect formation in enamel hypoplasia [13]. In Fallot Tetralogy, wrinkled tongue is observed as an oral finding [1].
Infective endocarditis
Infective endocarditis is a rare disease that results in high morbidity and mortality, with an annual incidence of 0.05- 0.12/1000 in children [3,14,15]. Turbulent blood flow observed in heart diseases leads to endothelial injury, resulting in storage of platelets and fibrin on the endothelial surface [15]. As a result, non-bacterial thrombotic endocarditis occurs and bacteremia results in the adhesion of bacteria to this injured endocardium and proliferation in vegetation leading to infective endocarditis. Therefore, some heart diseases pave the way for the development of infective endocarditis [14,15]. Invasive dental procedures, gastrointestinal and genitourinary systems related operations may cause bacteremia and infective endocarditis [15].
Bacteremia in dental procedures
In children, oral flora changes and streptococci (alpha hemolytic streptococci), actinomyces and privately species increase after infancy and begins to resemble adult flora. Healthy children have streptococci, staphylococci, neissera and haemophilus species, while older children have bacteria such as capnocytophaga and aggregatibacter actinomycetemcomitans, which cause periodontal disease [15]. The host’s response to dental plaque due to poor oral hygiene is gingivitis. When this inflammation develops, bacterial colonies may become involved in the gum capillary circulation due to thinning and ulceration. Therefore, there is a risk of bacteremia even in minimal procedures such as daily tooth brushing The frequency of bacteremia after toothbrushing and flossing has been reported to be 20-68%, 20-40% after tooth cleaning with toothpicks, 7-50% after mouth rinsing, and 7-51% after chewing food [3]. In addition, 10-100% after tooth extraction, 36-88% after periodontal surgery, 8-80% after removal of dental plaque, 9-32% after plastic matrix placement, 20% after endodontic procedures have been reported to develop bacteremia [3]. Good oral hygiene and prevention from diseases (such as gingivitis, tooth decay) are important to minimize the risk of bacteremia [15]. The use of amoxicillin in the selection of antibiotics in dental procedures has been shown to have a statistically significant effect on reducing the incidence and duration of bacteremia.
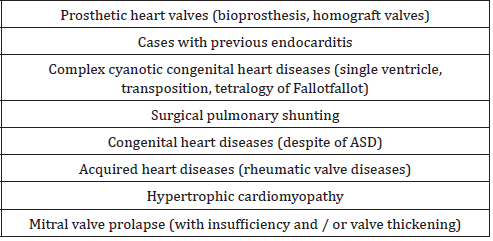
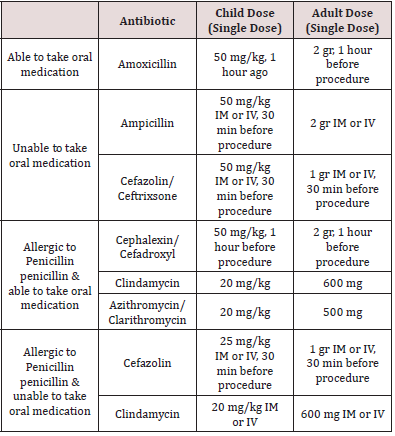
While previous American Heart Association (AHA) guidelines recommend antibiotic prophylaxis for all dental interventions that may cause bleeding, this recommendation has been altered since there is no evidence that this is a predictive symptom of bacteremia when bleeding occurs during dental procedures [3]. In the latest guidelines published by AHA, it was decided to administer prophylactic antibiotics only to the highest-risk group before invasive dental procedures [3] (Table 1). Prophylactic antibiotic administration is recommended only if high-risk patients are scheduled for an operation to the gingival tissue or the periapical region of the tooth, or if there is a risk of mucosal perforation. Routine injections of anesthetic agents, x-rays, removable dental prostheses, orthoses, orthodontic material placement, prosthesis matching, primary tooth extraction, antibiotic prophylaxis are not recommended in uninfected tissue [3]. Antibiotic prophylaxis should be given 30-60 minutes before the procedure. However, it can be given within 2 hours after the procedure if it is not given before the procedure [3]. In patients using oral anticoagulants, intramuscular injection should be avoided, and oral antibiotics should be preferred. Clindamycin, clarithromycin, azithromycin should be given to patients who routinely use antibiotics as they may be resistant to penicillin and ampicillin [3]. These patients should receive dental treatment 10 days after antibiotic treatment to normalize oral flora. In patients receiving intravenous antibiotic therapy, the antibiotic dose should be adjusted 30-60 minutes before dental intervention [3,16] (Tables 1&2).
Dentist approach
Patients with cardiovascular disease should be consulted with their doctors. Deciding on premedication, preoperative antibiotic requirements, anesthetic selection and surgical procedures should be decided in accordance with the recommendations of the physician of patient. In children diagnosed with cardiovascular disease, a preventive program including nutritional advice, fluoride therapy, fissure sealants and oral hygiene should be applied [1]. Arrhythmia due to endogenous catecholamines triggered by stress, fear and pain may develop during dental procedures, and patients who are prone to arrhythmia should be closely monitored [3]. Antibiotic prophylaxis should be performed in high-risk patients if a procedure is planned for the gingival tissue or the periapical region of the tooth, or if there is a risk of mucosal perforation [3]. Dental procedures in high and medium risk groups should not exceed the treatment of deep dentine caries. Direct pulp capping, pulpotomy and root canal treatments are not indicated because they increase the risk of bacterial endocarditis. In very deep decayed teeth, the treatment option should be extraction [1].
Conclusion
In children with cardiovascular disease, the risk of infectious endocarditis and bacteremia due to the risk of fatal outcome of the heart valve is very important in terms of oral and dental health in these patients. It is very important for dentists to consult with their physician before dental procedures in children with heart disease, and to take prophylaxis needs and stress tolerances of their patients by writing. These children and their families should be adequately informed about oral hygiene. In this way, the risk of bacteremia, even in oral cleaning procedures such as chewing and brushing, can prevent infective endocarditis [1].
Read More Lupine Publishers
Pediatric Dentistry Journal Articles: https://lupine-publishers-pediatric-dentistry.blogspot.com/

No comments:
Post a Comment